BY CHRISTINE KANNLER, MD, COMMITTEE ON ENVIRONMENTAL AND OCCUPATIONAL HEALTH MEMBER
Dr. Christine Kannler shares her motivations to advocate for occupational health screenings in this short video.
Illustration by Sioux Waks via Getty Images.

Dr. Christine Kannler
The US Preventive Services Task Force (USPSTF) aims to provide screening recommendations that help physicians enhance health outcomes and reduce cancer risk. Physicians utilize these guidelines daily to educate, screen, and treat their patients.
For example, the USPSTF recommends screening patients for obesity, tobacco usage, and alcohol consumption
— factors strongly linked to poor health outcomes.
However, the USPSTF recommendations do not address environmental exposures to known carcinogens in the workplace or home. Unlike tobacco and alcohol, which are widely understood by both patients and physicians, environmental exposures are often
unfamiliar to patients and not part of most physicians’ training. Consequently, systematic screening for occupational or environmental carcinogen exposure is uncommon, despite the well-documented risks these exposures pose to health.
Occupational Exposure
In recent years, there has been a growing understanding of the negative health impacts of environmental exposure as more research studies have been published and replicated in multiple cohorts. One of the most studied populations is firefighters.
In 2014, the National Institute for Occupational Safety and Health (NIOSH) studied 30,000 American firefighters and reported that they are nine percent more likely to be diagnosed with cancer and 14 percent more likely to die of their cancer.
Congress passed the Firefighter Cancer Registry Act in 2018, thereby enabling NIOSH and the Centers for Disease Control (CDC) to collect cancer data on firefighters nationally.
But firefighting is not the only occupation with elevated cancer risks. Police have an increased cancer mortality, although large-scale studies are needed. Coal miners, oil workers, gas field workers, and plastic production workers have an increased risk of leukemia, lymphoma, brain cancer, breast cancer, and mesothelioma.
Gardeners, landscapers, municipal workers, and horticulturists exposed to pesticides face elevated risk of leukemia, sarcoma, non-Hodgkin’s lymphoma, multiple myeloma, and Parkinson’s disease
.
Environmental Risks
More recently, there has been an increasing recognition that per- and polyfluoroalkyl chemicals (PFAS), which are widely used in products including nonstick cookware, waterproofing materials, and firefighter gear and foam, are associated with
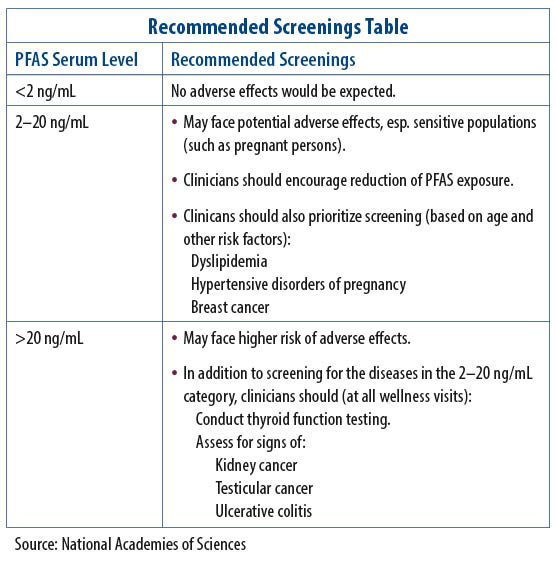
elevated cancer risk and poor health outcomes. In 2022, the National Academy of Sciences, Engineering, and Medicine (NAS) published clinical guidelines outlining when to screen the public for PFAS exposure, what blood test to order, and how to clinically follow patients for poor outcomes such as low birth weight, dyslipidemia, increased liver enzymes, thyroid dysfunction, ulcerative colitis,
kidney cancer, breast cancer, and testicular cancer.
However, few labs offer PFAS serum testing.* The Recommended Screenings Table below summarizes
NAS-recommended health screenings based on serum PFAS levels. Elevated levels can be reduced through blood or plasma donation, though PFAS in donations is not currently
monitored. A mechanism to discard PFAS-contaminated specimens is needed. The EPA is now screening municipal water for PFAS, emphasizing the need for physicians to screen exposed populations.
The Importance of Early Detection
Given the known adverse health risks of occupational risk factors, as well as the specific knowledge about environmental hazards, these factors provide an important and overlooked avenue for physicians to screen, detect disease, and initiate treatment
earlier. However, discussions about occupational or environmental exposures to known documented carcinogens are shockingly absent. The USPSTF currently has no health screening recommendations for documented environmental and occupational exposures,
such as PFAS in firefighting or petrochemical plants. Also, occupational and environmental exposures and their effects on health are not included in medical school curriculums and are rarely covered in residency programs or continuing medical
education programs.
Enhanced Detection Is Essential
Educating physicians about environmental exposure in screening is vital for earlier detection and better outcomes. Advances are significant, but effective care requires identifying at-risk individuals. Greater investment in prevention, early detection,
and public education on exposures is essential. Physicians should be trained to assess occupational and environmental risks, and the USPSTF should create exposure-based screening guidelines. Health insurers must cover early screening for exposed
individuals. Focusing solely on traditional risk factors like obesity, tobacco, and alcohol while ignoring environmental exposures is dangerously shortsighted.
*Providers can use test code 39307, ICD-10 code Z13.88, and CPT code 82542. The PFAS-REACH fact sheet addresses many pertinent questions such as which labs offer PFAS testing.
